Overview
In this section you will get an overview of the condition and its relevance to your health.
A vaginal yeast infection — medically known as vulvovaginal candidiasis — is one of the most common gynecological infections. Approximately 75 percent of all women develop one at least once in their lives, and many even repeatedly. Despite its prevalence, the condition can be very unpleasant for those affected.
Typical symptoms such as intense itching, burning, and discharge can significantly impair quality of life. At the same time, there is often uncertainty about whether it is actually a yeast infection or another type of infection.
The good news: A vaginal yeast infection can be treated easily and reliably in most cases. An online consultation can also be used to assess whether appropriate therapy is advisable.
What is it?
Here you will learn what medically characterizes this condition and how it is defined.
A vaginal yeast infection is usually caused by yeast fungi of the genus Candida, most commonly Candida albicans. These fungi naturally occur on the skin and mucous membranes and are normally harmless.
However, when the natural vaginal environment is disrupted, the fungi can multiply strongly and cause symptoms. Unlike bacterial vaginosis, this is a true inflammation of the vaginal mucosa.
It is important to distinguish this from other vaginal infections, as the cause, treatment, and course differ significantly.
Causes
The following information explains which factors can contribute to the development of this condition.
The development of a vaginal yeast infection is promoted by various factors that disrupt the natural balance of the vaginal flora.
Antibiotic use is one of the most common causes. Antibiotics reduce not only pathogenic bacteria but also protective lactic acid bacteria.
Hormonal influences also play a role. Pregnancy, hormonal contraception, or hormonal fluctuations during the cycle can promote fungal growth.
Other risk factors include:
- Diabetes mellitus, especially with poor blood sugar control
- Weakened immune system
- Tight, non-breathable clothing
- Excessive or aggressive intimate hygiene
A vaginal yeast infection is not a classic sexually transmitted disease but can be transmitted during intercourse.
Symptoms
This section describes the typical signs and symptoms you should watch for.
The symptoms of a vaginal yeast infection are usually pronounced and easily noticeable.
Typical complaints include:
- Intense itching in the vaginal and vulvar area
- Burning, especially during urination or intercourse
- White, crumbly discharge ("cottage cheese-like")
- Redness and swelling of the external genitalia
Unlike bacterial vaginosis, the discharge is usually odorless or only slightly acidic.
Warning signs that should be medically evaluated:
- Fever
- Lower abdominal pain
- Bleeding
- Recurring infections (more than four per year)
Diagnosis
Below you will learn how this condition is detected through medical examinations.
The diagnosis of a vaginal yeast infection is made through a gynecological examination and assessment of typical symptoms.
A vaginal swab can detect the fungal pathogen microscopically or in the laboratory and is particularly useful for unclear or recurring symptoms.
Important: Not every itch in the intimate area is a yeast infection. A correct diagnosis prevents incorrect treatment.
During an online consultation, symptoms and pre-existing conditions can be assessed. For typical symptoms, therapy can be initiated or a gynecological examination recommended.
Treatment
Here the available therapy options and their modes of action are explained.
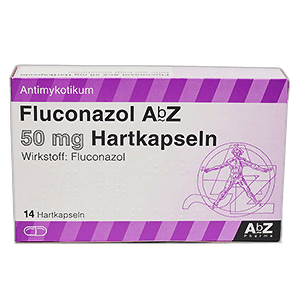
Treatment of a vaginal yeast infection is with so-called antifungals.
Clotrimazole is a commonly used active ingredient for local treatment. It is applied as a vaginal tablet, cream, or combination product and acts directly against the fungi. Side effects are usually mild and limited to local irritation.
Fluconazole is an oral antifungal that is often used as a single dose. It works systemically and is particularly useful for severe or recurring infections. Possible side effects include gastrointestinal complaints or headache.
Important notes:
- Therapy should be completed consistently.
- Intercourse should be avoided during treatment if possible.
- The partner generally does not need to be treated, unless symptomatic.
For recurring vaginal yeast infections, longer-term therapy may be necessary.
Available medications
Various prescription medications are available for treatment. Click on a medication to learn more about its effects, dosage and side effects.
Prevention
This section provides guidance on prevention and reducing risk factors.
To prevent vaginal yeast infections, gentle care of the intimate area is essential.
Recommended measures include:
- Breathable cotton underwear
- Avoiding aggressive soaps and intimate sprays
- Gentle intimate hygiene without vaginal douching
For known risk factors such as diabetes, good management of the underlying condition is important.
FAQ
Here you will find answers to frequently asked questions on this topic.
Would you like a medical assessment?
Fill out the medical questionnaire. A licensed doctor will review your information and recommend a suitable therapy if appropriate.
Important notice
This content is for general information only. In case of severe pain, shortness of breath, impaired consciousness, fever > 39°C or rapidly worsening symptoms, please seek immediate medical help ().
Related treatments
More treatments from the Frauengesundheit area that might interest you.
Verhütung
Ein kurzer Check der wichtigsten Eckdaten – danach kann eine passende Option ausgewählt werden.
Gesichtsbehaarung
Wir stellen ein paar gezielte Fragen, um mögliche Ursachen und passende Optionen einzuordnen.
Bakterielle Vaginose
Ein kurzer Fragebogen hilft, typische Beschwerden und mögliche Ausschlusskriterien abzufragen.
Blasenentzündung
Wir prüfen Symptome und Warnzeichen, damit eine passende Empfehlung medizinisch sicher eingeordnet werden kann.